Strange as it may seem, less than half your body is human.
57% of the cells in you body are bacteria, viruses, fungi, and a type of single-celled microorganism you’ve probably never heard of, called archaea. Together they make up the microbiome.
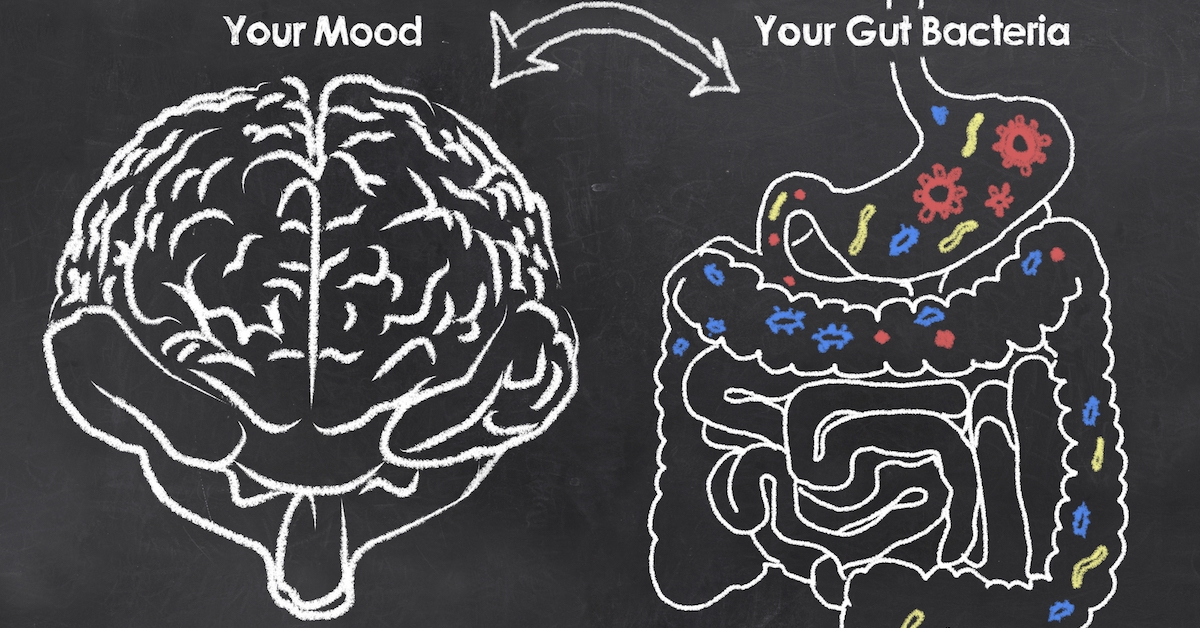
Evidence has been mounting over the last 25 years that the microbiome (particularly those organisms in the intestines) can protect us from – or cause us to fall victim to — a wide range of health problems, including those affecting the brain.
This is a hot research area. Today, many scientists believe we are on the brink of a mind revolution, whereby “mood microbes” or “psychobiotics” could be prescribed for mental health disorders. This is fascinating and important stuff. . .
Gut Bacteria Produce Brain Chemicals
The study that sparked the interest of scientists came out of Japan in 2004.
In their experiment, germ-free mice, with no microbes at all living in their bodies, were found to produce twice as many stress hormones as normal mice when subjected to the same upsetting conditions. This strongly suggested that bacteria could affect the brain.
They do so by way of the vagus nerve, which runs from the abdomen to the brain. This is a neurological super highway between your colon and the organ between your ears. Not very flattering, but a healthy poop factory is essential to a healthy brain.
The microorganisms in the intestine act on the villi – tiny finger-like projections in the intestinal wall. These send electrical impulses along the vagus, through the blood-brain barrier, and into brain structures.
Probiotics for a Better Mood
The gut microbes produce a wide range of hormones and neurotransmitters like GABA, dopamine and serotonin to regulate digestion, appetite and feelings of fullness. These same chemicals can travel to the brain to influence our mood. You’ve probably heard of serotonin, which the psychiatric profession is so focused on when it comes to treating depression.
The other neurotransmitters are just as important.
At the University of Cork in Ireland, scientists fed mice a broth containing Lactobacillus rhamnosus. This bacterium, common in over-the-counter probiotic supplements, occurs naturally in humans and is able to release large quantities of nerve-calming GABA.
The research was led by neuroscientist John Cryan, who’s a full professor and department chair at Cork U. He summed up the effect of the broth on the mice: “They behaved as if they were on Prozac. They were more chilled out and more relaxed.”
In other words, the right bacterium is as powerful as a pharmaceutical depression drug. And I’ll wager it’s a lot safer.
Linked to Depression and Parkinson’s
In a later study by the same group, the microbiome from patients suffering with depression was transferred to rodents through a procedure called a fecal microbiota transplant (FMT). The researchers found that the creatures also became depressed. (Just by way of a sidelight, fecal transplants are gaining support as a medical treatment for humans.)
Prof, Cryan’s colleague, pharmacologist and professor of psychiatry Ted Dinan, observed, “We were very surprised that you could, just by taking microbiome samples, reproduce many of the features of a depressed individual.”
One of these features was anhedonia, where there is a loss of interest in activities the patient used to enjoy. Rats usually love sugary water, but after receiving a fecal transplant from a depressed human, they lost all interest.
People who suffer from depression have a less diverse microbiome. Prof. Dinan believes this plays a role in causing the condition for many people.
Parkinson’s disease is likewise one of the diseases linked to a less diverse microbiome.
Prof. Sarkis Mazmanian, a medical microbiologist from the California Institute of Technology, found large differences between the microbiome of those with the brain disease and those without.
Mice receiving bacteria from Parkinson’s patients by way of a fecal transplant developed symptoms that were “much worse” compared to mice receiving a transplant from healthy people.
In Prof. Mazmanian’s view, “The changes in the microbiome appear to be driving motor symptoms; appear to be causal to the motor symptoms. We’re very excited about this because it allows us to target the microbiome as an avenue for new therapies.”
Dr. Christopher Coe, Director of the Harlow Center for Biological Psychology at the University of Wisconsin-Madison, said it was plausible “we might one day use microbes to diagnose neurodevelopmental disorders, treat mental illnesses and perhaps even fix them in the brain.”
Meanwhile, Create Your Own Healthy Microbiome
A healthy microbiome is diverse, carrying many different species.
And good news, it’s possible to change it for the better, quickly. You can experience measurable changes within 24 hours of changing the way you eat. Our diets have a huge impact.
Eating many different kinds of fibrous fruits and vegetables will give your gut bacteria something to chew on.
Some sources of fiber are particularly helpful in boosting good bacteria, such as onions, leeks, garlic, chicory, dandelion greens, Jerusalem artichoke, asparagus and bananas. Other good sources of fiber are barley, oats, flaxseed, apples and seaweed.
Certain types of starch resist digestion and feed bacteria. These are found in grains, legumes and seeds.
You can also top up your good bacteria with probiotic foods like yogurt, non-processed cheeses and fermented foods such as sauerkraut, kefir and kimchi.
- http://www.bbc.co.uk/news/health-43815370
- https://www.nytimes.com/2015/06/28/magazine/can-the-bacteria-in-your-gut-explain-your-mood.html
- The Clever Guts Diet by Dr Michael Mosley. Short Books, 2017